Dr. David Rawlings knows how painful and devastating malaria is—he had it several times in his early 20s while teaching grade school in Kenya.
“It’s a horrible infection,” said Rawlings, director of the Center for Immunity and Immunotherapies at Seattle Children’s Research Institute. “I had a high fever, severe headaches, chills and I couldn’t leave my house for days. I was fortunate to have medications that stopped the infection, but malaria these days is resistant to most of these drugs.”
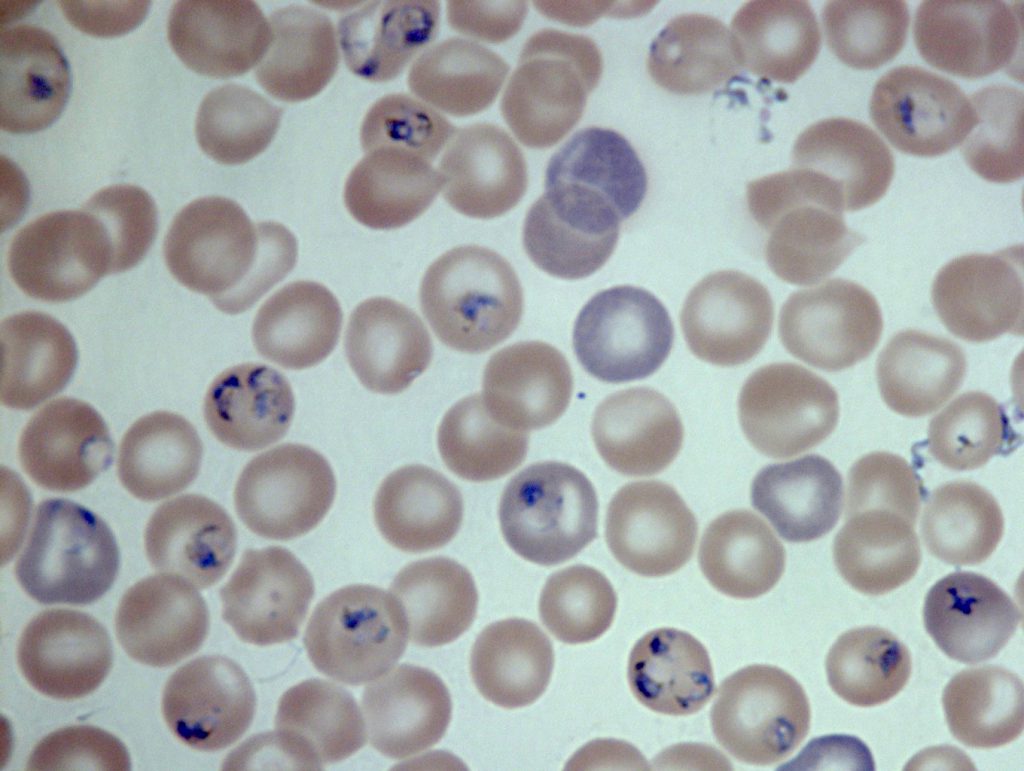
Rawlings recovered from the bouts of malaria, but young children who get malaria are not always so lucky. According to the Centers for Disease Control and Prevention, 214 million cases of malaria occurred worldwide in 2015 and resulted in 438,000 deaths, most of them children in Africa. The disease is a parasitic infection spread through the bite of infected mosquitos.
Seeing his young students in Africa come down with malaria is what pushed Rawlings to become an immunologist. He wanted to find a cure.
Today, researchers at the University of Washington and Rawlings’ lab at Seattle Children’s revealed a major breakthrough in malaria immunology research that they describe in a study published in the journal Immunity.
“The search for an effective malaria vaccine has been a vexing scientific problem for decades,” Rawlings said. “But now we’ve identified a population of antibody producing cells that may be key to developing a more effective vaccine.”
Remarkable results with an overlooked immune cell
Lead authors Dr. Marion Pepper and Akshay Krishnamurty of the University of Washington partnered with Rawlings and Dr. Chris Thouvenel at Seattle Children’s Research Institute to discover the power of an immune cell that researchers had not considered previously in vaccine development.
Vaccines for diseases like the flu, chickenpox and measles mimic the infection in the body to kick the immune system into action. When a person receives a vaccine, the immune system ramps up and triggers the development of antibodies, which stay in the body and fight any future infection.
All the common vaccines are based on getting one particular immune cell, the IgG memory B cell, to stimulate a strong immune response and produce massive amounts of antibodies.
“Researchers have relied on IgG memory B cells in vaccines because they do a good job producing a strong antibody response,” Pepper said. “But we found that IgM memory B cells multiply more rapidly and produce higher amounts of antibodies than IgG memory B cells early after re-exposure to infection.”
Rawlings adds that this finding could help solve the riddle of why an effective malaria vaccine has eluded scientists.
“To induce a robust immune response that protects against malaria, we have to find the best memory B cell for the job,” he said. “With IgM memory B cells, we’ve identified a malaria antibody powerhouse.”
Having singled out the memory B cell in mouse malaria that holds promise for malaria vaccine development, Rawlings and Pepper are moving the work closer to human application by studying the antibodies in blood samples directly from patients who have survived multiple malaria infections.
This knowledge will help guide vaccine design and identify antibodies that could be produced in large quantities, which could then be passively transferred to people to protect them from disease or help them control an ongoing infection.
Ending the painful cycle of malaria

According to the World Health Organization, children under 5 years of age are one of the most vulnerable groups affected by malaria. In areas with high rates of malaria, the deadly side effects of severe anemia, hypoglycemia and cerebral malaria are seen more often in children.
“Malaria is tough on children’s developing bodies because it’s an infection they can acquire again and again,” said Rawlings, who is also a professor of pediatrics at the University of Washington. “Even if they can get through the cycles of the disease and through the long recovery, bouts of malaria severely disrupt physical and social development.”
Pepper and Rawlings believe that their findings will fundamentally shift the scientific understanding of malaria vaccine development and could hold broader implications for vaccines.
“This finding challenges the current understanding of which immune cells may be most effective in vaccine development,” Pepper said. “This is an important finding for malaria, and it may prove to be useful in developing other vaccines.”
Resources
- Study in Immunity: Somatically Hypermutated Plasmodium-Specific IgM+ Memory B Cells Are Rapid, Plastic, Early Responders upon Malaria Rechallenge
- Dr. David Rawlings, Seattle Children’s Research Institute
- Dr. Marion Pepper, University of Washington
- Malaria, World Health Organization

