Ellie Musgrave found her calling when she was 4 years old. Her father took her to the racetrack and a dream sparked. She surprised her dad by saying, “I want to do that.” Much like the electrical charge that brings a car to life, the draw to racing happened in an instant and throttled her […]
When Ryder Gordon was 2 years old, he underwent his first surgery. It took 12 hours and saved his life. Thomas Gordon and his wife, Magi, vividly remember the day they handed over their son to surgeons at Seattle Children’s. “It was gut-wrenching,” said Magi. “You want more than anything to switch places with your […]
Just in time for Autism Acceptance Month, the Seattle Children’s Alyssa Burnett Adult Life Center (ABC), which offers lifelong learning for people 18+ with autism spectrum disorder (ASD) and other developmental disabilities, reopened its expanded doors in late March, rolling out in-person classes for the first time since the COVID pandemic began.
Epilepsy can be very difficult to treat – and some families explore a range of options seeking relief from seizures for a child with epilepsy looking for a solution. For 14-year-old Taylor Johnson, a procedure known as deep brain stimulation (DBS) resulted in her experiencing a completely new life and the significant seizure relief she […]
Sirish was a healthy, happy boy with no underlying medical conditions aside from food allergies and eczema, both of which were easily managed at home. Then one day, he spiked a fever. Initially, his mother, Jyothi, a physician who previously practiced in India, wasn’t concerned. The fever broke, and Sirish seemed to improve. About a […]
New research and treatments for epilepsy have come a long way in the last several years. In this Q&A, we talk with Dr. Edward “Rusty” Novotny, director of Seattle Children’s Epilepsy Program and professor of neurology and pediatrics at the University of Washington. As the director of one of the largest epilepsy programs in the […]
As a high school freshman, Liesel Von Imhof had a dream of attending college at Harvard. She packed her schedule with challenging classes and participated in varsity sports such as cross-country running and cross-country skiing. She had occasional, debilitating headaches that sometimes caused her to miss school, but she blamed them on stress, dehydration or […]
Updated March 4, 2022: Thank you to our community of donors for your outpouring of sympathy, support and interest in celebrating the life of patient Zain Nadella, who recently passed away. Zain was the beloved son of Anu and Satya Nadella, and as a long-time patient, the family considered Seattle Children’s a second home. We […]
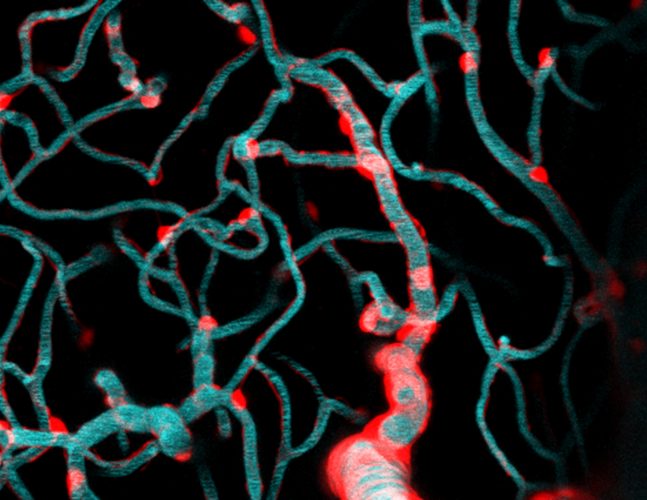
While the human brain has over 400 miles of total vasculature, little is known about the tiny capillaries that make up much of this intricate labyrinth of blood vessels critical for delivering oxygenated blood and nutrients to billions of brain cells. According to Dr. Andy Shih, a principal investigator in the Center for Developmental Biology […]
When 11-year-old, Giorgia Graham, told her parents her cheek was going sporadically numb, they thought it was because she banged her face playing tag. But when the numbness kept coming back, her parents realized it was something more serious. They discovered Giorgia was having seizures when she experienced a grand mal seizure sleeping one night […]