Colleen and Derek spent the first half of Colleen’s pregnancy like many first-time parents, imagining what their child would be like, musing about things they would do as a family and celebrating a joyful new chapter in their lives. They never imagined they would have a child with special needs or that doctors would predict […]
When a pregnant Heather Henson learned her baby, Dawson, had hypoplastic left heart syndrome — a rare and serious condition where the left side of the heart is not fully developed — she immediately began researching the disease and the hospitals that treat it. Heather and her family live in Anchorage, Alaska. The state doesn’t […]
“Before COVID-19 restrictions, patients facing surgery were given the opportunity to tour the hospital with their families ahead of time to help ease the nerves and to become comfortable with the process. Since that option became unavailable, Dr. Henry Ou took it upon himself to create a virtual tour that a kid can walk through […]
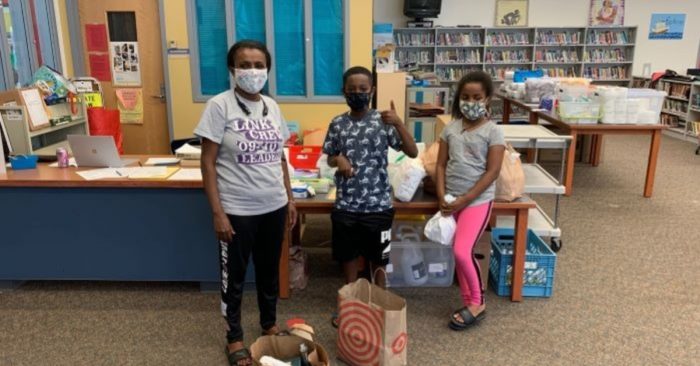
When the economic and social impacts of the coronavirus pandemic began taking root in early spring 2020, the team at Seattle Children’s Odessa Brown Children’s Clinic (OBCC) immediately anticipated the devastation and hardship it would bring. “From the start, we recognized that the families we serve were being disproportionally negatively impacted by the virus itself, […]
The U.S. Food and Drug Administration on Feb. 5 approved Bristol Myers Squibb’s Breyanzi, a chimeric antigen receptor (CAR) T-cell therapy used to treat adults with certain types of large B-cell lymphoma who have not responded to or who have relapsed after standard treatments. The approval was supported by research at Seattle Children’s, including the […]
Doctors at Seattle Children’s are investigating whether a simple liquid biopsy containing a small amount of fluid from a patient may someday provide an easier route to a genetic diagnosis in children with vascular or lymphatic malformations. The work is a collaborative effort led by Dr. James Bennett, a clinical geneticist and co-director of the […]
When 11-year-old, Giorgia Graham, told her parents her cheek was going sporadically numb, they thought it was because she banged her face playing tag. But when the numbness kept coming back, her parents realized it was something more serious. They discovered Giorgia was having seizures when she experienced a grand mal seizure sleeping one night […]
Before his first breath, Colton Iverson had already received the gift of a lifetime. Just days old, he became the youngest patient to go on a drug recently approved by the U.S. Food and Drug Administration (FDA) for the treatment of a life-threatening genetic condition called very long-chain acyl-CoA dehydrogenase, or VLCAD, deficiency. For his […]
It’s been over three years since Maxford Brown woke up one morning not feeling well. Neither Maxford nor his family had any idea that it would mark the beginning of a life-changing journey with a rare, but serious neurological condition called acute flaccid myelitis, or AFM. “I suggested it might help for him to lay […]
An international panel of sleep experts is adding a new pediatric sleep disorder they call restless sleep disorder, or RSD, to parents’ and pediatricians’ radars. Led by Seattle Children’s pediatric sleep specialist, Dr. Lourdes DelRosso, the group shares their consensus on a medical definition of RSD in a new paper published in Sleep Medicine. Known […]