Transplant day is a joyous milestone for children and families who’ve been through a difficult illness. But the healing does not end when the new organ is in place—in fact, that is when the real work begins, according to Dr. Jodi Smith, Medical Director for the Kidney Transplant Program at Seattle Children’s. “One of the […]
Aaden Adams remembers waking up in his room in the Cardiac Intensive Care Unit (CICU) at Seattle Children’s Hospital and asking for red Popsicles. “Everybody wanted me to talk and I wanted a red Popsicle,” said the precocious 6-year-old with a face full of freckles. “So I asked for Popsicles. Do you remember that, Mom?” […]
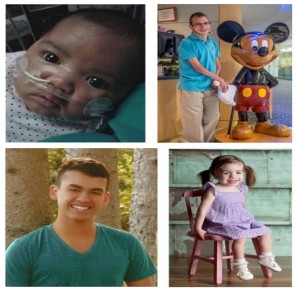
Parker Rana, 15, has truly overcome the odds to get to where he is today. Born with multiple heart defects, Parker grew up in and out of the hospital. But now, he’s a thriving teenager with an incredible story of hope. Below is Parker’s story: from hospital bed to trackside, cheering on his favorite racing […]
April marks National Donate Life Month, a time devoted to spreading awareness about the tremendous need for increasing the number of organ, eye and tissue donors. According to the United Network for Organ Sharing (UNOS), more than 120,000 people in the U.S. are on the waiting list for a lifesaving organ, and sadly, more than […]
The language of medicine is full of complicated words and acronyms. For parents of children with serious heart conditions like congenital heart disease or pulmonary hypertension, one such acronymn that may incite fear or worry is hearing that their child may need a device called a VAD (Ventricular Assist Device). However, these devices, combined with […]
It can be hard enough to remember to take a multivitamin every day; imagine having to take 20 pills at specific times throughout the day, every day, for your whole life. That’s the reality individuals who have undergone an organ transplant must face. In order to stay healthy and to keep their bodies from rejecting […]
Kami Sutton, 26, who you met last week, has been waiting for a heart transplant for five years. But surgeons at Seattle Children’s and University of Washington Medical Center (UWMC) are now preparing to perform a difficult surgery that could greatly improve her quality of life and may even eliminate her need for a transplant. […]
Children who need a heart transplant face a frightening waiting game before a donor heart becomes available. They must live with a failing heart for months, or even years, as clinicians strive to keep them healthy enough for transplant. Nationally, these patients face the highest waiting list mortality in solid-organ transplantation medicine, with 17% of children […]
As we head into the New Year, we’d like to reflect on some of the incredible clinical advancements of 2014 that show how our doctors have gone the extra mile for our patients. In the Children’s HealthLink Special video above, watch how futuristic medicine has saved the lives of the littlest patients at Seattle Children’s. From 3D-printed heart models to liquid ventilation, doctors […]
In honor of the New Year, we’re taking a look back at some of our most popular and memorable blog posts from 2014. Below is a list of our top 10 posts. Here’s to another great year of health news to come. Happy New Year! Lung Liquid Similar to One Used in Movie “The Abyss” […]