Last spring, Wesslee Holt rolled his ankle at his middle school in Shelton, Washington. The 12-year-old is a dedicated member of his cheer team and was eager to return to the squad quickly. He followed his doctor’s instructions to immobilize the foot and wear a boot — but his pain only increased over time.
Wesslee started using a scooter to keep weight off his foot and rested it as much as possible. Nothing seemed to work. His skin became splotchy and red, and was so sensitive to touch that he couldn’t put a sock or shoe on. He felt depressed and anxious, pulled out of cheer team completely and even left school.
His mother, Steph Fyfe, knew it was time for a different approach. “People wanted to put Wesslee on supplemental security income and call him disabled, but I knew there had to be a way for him to get better,” she said.
She was referred to Seattle Children’s Pain Medicine Clinic and learned Wesslee was suffering from complex regional pain syndrome (CRPS), which sometimes accompanies a routine injury and causes the nerves to send extreme pain messages to the brain. The good news is that Seattle Children’s was able to offer Wesslee a unique treatment option: the Pediatric Pain Rehabilitation Program (PReP).
An intensive treatment with big results

As one of only nine pediatric programs of its kind in the country, the Seattle Children’s PReP team faces high demand for its services. Pain psychologist Dr. Karen Weiss attributes part of the group’s success to its innovative approach toward pain.
“For patients in chronic pain, it’s not a symptom — it’s a disease,” said Weiss. “With CRPS, evidence points to rehabilitation as the most effective strategy. In this setting, improving a child’s function leads to an improvement in their pain.”
Children and adolescents in the program participate in intensive outpatient therapy, usually for two weeks. They come to the hospital from 7 a.m. to 4 p.m. every day, typically spending five of those hours in physical and occupational therapy.
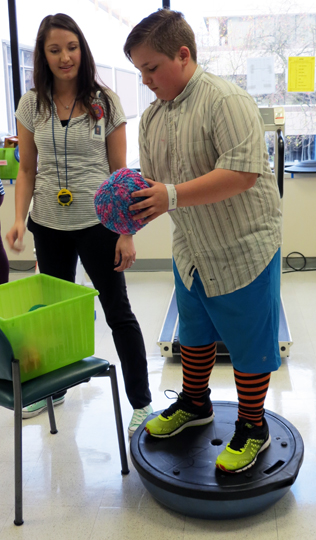
The therapists employ a great deal of creativity and compassion with participants — rolling humor, distraction and play together to make the “work” engaging.
One popular activity is bowling, where patients strengthen their core by launching a yarn ball at bowling pins using only their legs and a slingshot made of an exercise band. Patients love it — and they make tremendous progress in the context of fun.
The rest of the time is spent with other providers on the team: a nurse practitioner who oversees the medical side of treatment; a social worker who gauges the effect of the pain on parents and families; a teacher who helps students keep up with school work; and Weiss, a pain psychologist who focuses families on coping skills and behavioral changes that support increased functioning.
Weiss says the treatment is intense and effective. She teaches children coping skills like deep breathing, muscle relaxation and imagery — as well as how to use positive thinking to persevere during difficult exercises.
Patients who are referred to the program have typically experienced long bouts of chronic pain from conditions like juvenile idiopathic arthritis, chronic headaches, abdominal pain or — like Wesslee — CRPS. Their therapy requires a great deal of motivation and commitment because they have to learn to cope with pain, not just wait for it to go away. “Our goal is to see kids walk out and return to their full range of activities, and we see astounding progress,” said Weiss.
Wesslee can certainly attest to the effectiveness. When he entered the program, he hadn’t used his leg in more than three months — but three weeks later, he walked out of the hospital and back to his cheer team.
Small steps, big success

Within days of starting the PReP program, Wesslee was able to put on a shoe and walk with a crutch. His therapists employed lots of tools and tactics in the rehabilitation gym, but they also used the entire hospital environment — inside and outside — as their therapy space.
“We worked with Wesslee in real-life environments, like the hallways, stairwells or out on the sidewalks,” said physical therapist Sharon Yurs. “He found the therapy to be challenging — but whatever we asked him to do, he always persisted with his effort.”
Fyfe was with her son every step of the way and remembers a turning point in his treatment. “He had a goal to walk to the therapy pool and he really wanted to do it on his own,” she said. It took Wesslee 45 minutes to make the trek across the hospital.
One employee stopped to ask if they needed anything, and when Fyfe said they were in the PReP program, the employee immediately understood. “She went ahead of us, and when we got to the zone where the pool is a group of staff members were waiting for us — cheering Wesslee on,” Fyfe said. “They followed us the rest of the way, clapping and celebrating his progress. That person’s outreach really made a difference.”
After his therapy, Wesslee added a new goal to his list: pursuing a career as an occupational or physical therapist. “He saw what this amazing group of people can do and he wants to help other people work through their challenges,” said Fyfe.
Wesslee says the therapy was challenging, but it got easier once he realized he could do the things his therapists were asking of him.
When asked what he would say to other children and teens who are entering the PReP program, Wesslee’s advice is clear. “Do it,” he said confidently. “Just push through — it’ll get better.”

