
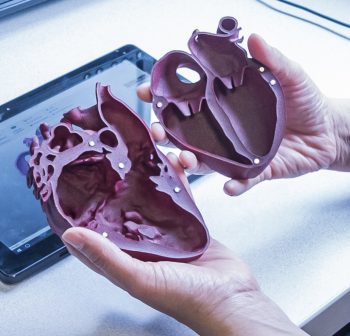
Rachael Satake holds a 3D-printed replica of her son’s heart condition in her hands during a recent appointment at Seattle Children’s Heart Center. For the first time since learning about the defect midway through pregnancy, she clearly sees how the surgeries he has undergone are helping his heart work despite having only one ventricle.
Her son, Auren, has a serious congenital heart defect called hypoplastic left heart syndrome (HLHS), which means he was born missing the left ventricle of his heart. His right ventricle works double time to supply blood to both his lungs and the rest of his body.
Babies with HLHS undergo three surgeries to help restore the function of their heart. The first surgery usually takes place by the time the baby is 10 days old. The third surgery is typically completed before the child’s fifth birthday. At 17 months, Auren is currently between his second and third surgeries.
“With the complexity of Auren’s treatment, it’s really important that as a parent I can understand what’s going on as much as possible,” Satake said. “It’s a lot of technical information to process. Everything made so much more sense when I saw the 3D model.”
New study uses printed and digital 3D hearts

The 3D-printed heart Satake used in the appointment is a part of a new research study at Seattle Children’s exploring the use of printed and digital 3D models to improve physician communication with parents and patients about their heart disease.
Dr. Sujatha Buddhe, a pediatric cardiology imaging specialist in the Heart Center and researcher in the Center for Clinical and Translational Research, is leading the study. She hopes the 3D models will offer improvement over the 2D drawings cardiologists and surgeons use to explain complex heart disease, congenital heart defects and surgical procedures to families. The study received support for this pilot study through Seattle Children’s Pediatric Pilot Fund.
“We’re trying to present this complex information to parents who are already stressed out with a diagnosis of something being wrong,” Buddhe said. “It’s difficult for them to develop a real understanding of what’s happening with their child’s heart when all they have to rely on are random pen and paper drawings.”
The making of a 3D heart
Buddhe collaborated with colleagues, including Seth Friedman in Radiology and Chris Howard in the Imagination Lab at Seattle Children’s, to develop the initial prototypes for the study. To make the models as realistic as possible, they converted computed tomography and magnetic resonance imaging scans of actual patient hearts into 3D images.
“A lot of time went into making the models specific to the types of heart disease we treat,” she said. “We simplified the detailed 3D models we use to plan surgeries, so that our models for patients and families clearly show the heart disease.”
The team tested different sizes and materials before producing a bank of 20 congenital heart disease models that are now available at the Heart Center cardiology clinics. At four times the size of an actual infant heart, parents and patients can hold the hard plastic models in their hands. The models easily open to show the inner chambers of the heart.
Similarly, Buddhe used the same 3D images to develop a digital version of the printed model. Shown to families on a handheld tablet, the cardiologist or surgeon can rotate the image on the screen to show different views of the heart. Buddhe said it’s possible to email these images to the family after the appointment, a benefit the digital hearts offer over their 3D-printed companions.
A transformative approach to patient education

Even though Satake learned as much as she could about HLHS through Seattle Children’s Prenatal Diagnosis and Treatment Center before Auren was born, she found it difficult to grasp all of the medical information.
“We’re extremely grateful to everyone at Seattle Children’s, from our prenatal doctor to Auren’s surgeons, doctors, nurses and therapists, for spending so much time with us to make sure we understand as much as possible,” she said. “Still, there are times when it’s hard to wrap my head around everything. I’m a hands-on learner, so being able to hold and even manipulate something makes a world of difference in my comprehension.”
Dr. Titus Chan, a cardiologist in Seattle Children’s Single Ventricle Program, immediately saw the value in showing Satake the 3D-printed models in their recent appointment. He used both a normal heart model and a model of HLHS to illustrate the differences in Auren’s heart. He said drawings tend to simplify the complex procedures. On the other hand, the 3D models may help convey the full extent of the patient’s heart disease.
“Rachael is very well-versed in Auren’s heart disease, so it was striking to hear how helpful the model was to her at this stage even though she is very familiar with his condition,” he said. “It’s really transformative to hold up a normal heart next to a replica of that patient’s heart disease. It gives families the opportunity to understand how different their child’s heart is and why.”
What’s next?
Parents and patients aren’t the only ones Buddhe believes will benefit from the new 3D models. She anticipates that the models will also help medical students and nurses, especially those in the intensive care setting who take care of pediatric heart patients after surgery.
At Seattle Children’s, 3D-printed models are already assisting surgeons in planning for complex or novel surgical procedures. The Heart Center team is also collaborating with Pear Med, a startup in the University of Washington’s CoMotion Labs, to produce patient-specific 3D heart models in an interactive virtual reality setting to not only assist surgeons in planning for surgery, but also potentially aid in patient family education.
“Virtual reality is the newest technology we’re exploring for surgical training and patient education,” said Dr. Jonathan Chen, chief of pediatric cardiovascular surgery and co-director of the Seattle Children’s Heart Center. “It’s possible we can bring virtual reality headsets and controls to the bedside, giving the surgeon the ability to lead parents through a virtual model of their child’s heart.”
Such technology, he said, will help transcend a knowledge gap in explaining everything from the most common congenital defects to the most complex congenital heart disease.
“I’ve always felt that Seattle Children’s does an amazing job caring for Auren while also taking really good care of me and my husband,” Satake said. “It means a lot that they are investing in technology for the parents’ well-being as much as the child’s.”
Her feedback provided in a short questionnaire about the 3D model will guide the Heart Center in determining if patients and families learn better with the 3D-printed or digital heart models.
“I’m pretty excited they decided to make the 3D models,” she said. “It would have been incredibly helpful to have that information from the very beginning during my prenatal care.”

