Antibiotics improve our lives in innumerable ways, but there is growing concern that their overuse is increasingly exposing the public to drug-resistant bacteria. Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die as a direct result of these […]
Each year in the United States alone, 20,000 children under the age of 5 are hospitalized due to complications from the flu. In 2014, influenza claimed the lives of more than 140 children; half of whom were healthy and had not been vaccinated. “It’s important for everyone – especially children – to get a flu shot […]
Many kids can relate to the unpleasant experience of growing pains – they come on at night and can cause sharp, shooting, as well as dull and nagging pain. But what people may not know is what causes them, why do they affect some children and not others, and most importantly, when should parents be […]
Imagine living every day of your life waiting for your child to have their next seizure. This is often the reality for parents of children with intractable epilepsy – a chronic form of epilepsy that can’t be controlled by medications alone. Every moment is plagued by uncertainty, and the world quickly becomes a place filled […]
They say that life is all about the little things, and for the Otolaryngology care team at Seattle Children’s Hospital, this statement holds true more often than not. Each year more than 150 children find their way to the Seattle Children’s Otolaryngology clinic to have some kind of household object, or “foreign body,” removed from […]
It’s no secret that traffic congestion is a problem in Seattle. If it feels like it has gotten worse lately, it’s not just you. A new study released last week by the Puget Sound Regional Council found that delays on regional freeways have gone up by more than 52% since 2010. Seattle already has the […]
Last month, TIME reported on the death of a 32-year-old Taiwanese man who suffered heart failure after an apparent three-day video game binge. Over the past several years similar stories have come to light, and as the scientific research into the effects of video games on the brain continues to increase, many parents may be wondering just […]
When it comes to the holiday season, sugar is everywhere, particularly in desserts and holiday candy. But did you know that sugar is also added to many everyday foods, including soups and yogurt? “Many people are unaware of just how pervasive added sugar is in our foods,” said Dr. Mollie Grow, a pediatrician at Seattle […]
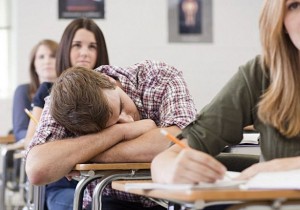
New data suggests that adolescents in the U.S. are chronically sleep-deprived. Doctors recommend the average teenager get between 8.5 to 9.5 hours of sleep on school nights, but a recent study conducted by the National Sleep Foundation found that 87 percent of high school students were sleeping far less. That’s a real concern for parents […]
On a Saturday in March, 13-year-old Trey Lauren was playing with his friends at a birthday party when he fell and cut his knee on a nail. It was a typical injury for a kid his age, but what resulted was anything but typical. Trey was taken to a local emergency room that night, and […]