Dr. Sandra “Sunny” Juul recently became the new Division Chief of Neonatology at Seattle Children’s Hospital and the University of Washington, taking the helm from Dr. Christine Gleason, who stepped down to pursue other professional goals. Below, Juul talks about her vision for her own research and for the Division of Neonatology at Seattle Children’s. […]
As we head into the New Year, we’d like to reflect on some of the incredible clinical advancements of 2014 that show how our doctors have gone the extra mile for our patients. In the Children’s HealthLink Special video above, watch how futuristic medicine has saved the lives of the littlest patients at Seattle Children’s. From 3D-printed heart models to liquid ventilation, doctors […]
In honor of the New Year, we’re taking a look back at some of our most popular and memorable blog posts from 2014. Below is a list of our top 10 posts. Here’s to another great year of health news to come. Happy New Year! Lung Liquid Similar to One Used in Movie “The Abyss” […]
Elise Pele had been in labor for hours awaiting the arrival of her baby girl, Tatiana, on the evening of Aug. 29. Elise remembers wanting desperately to hear her baby cry – a sign that everything was ok. But that cry never came. She saw Tatiana for only a few seconds before nurses rushed her […]
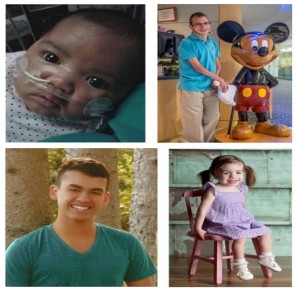
When you see pictures of tiny preterm babies, you likely marvel at how they fit in the palm of a hand, or how a wedding ring can slide up their arm and reach their elbow. What you may not consider is the lifelong toll premature birth can have on a person – if they survive […]
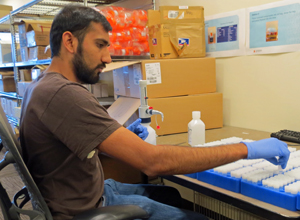
What does a pregnant woman in Yakima have to teach a researcher at St. Louis University? How can a Seattle woman’s healthy, full-term pregnancy impact future pregnancies in Europe or Africa? The answers are closer than you might think. Over the past seven years, the team at the Global Alliance to Prevent Prematurity and Stillbirth (GAPPS) – an […]
The following is part 2 of our two-part series on ECPR, a combination of CPR and ECMO offered at Seattle Children’s Hospital to save the most fragile patients’ lives. Part 1 covered Hannah Mae Campbell’s incredible story where ECPR and a heart transplant saved her life and allowed her to be the thriving toddler she […]
Shortly after Julie Wyatt delivered baby Nolan Wyatt on December 15, 2013 in Olympia, she received some startling news. Nolan was diagnosed with a congenital diaphragmatic hernia (CDH) – a hole in his diaphragm – a potentially life-threatening condition. It was something they didn’t see coming. Typically, CDH can be diagnosed before birth using an […]
The following is part 1 of a two-part series on ECPR, a combination of CPR and ECMO offered at Seattle Children’s Hospital to save the most fragile patients’ lives. Here, we tell Hannah Mae Campbell’s story and how ECPR saved her life. In part 2, we’ll discuss how Seattle Children’s has spearheaded a first-of-its-kind ECPR […]
Complications that can arise around the time of birth may reduce oxygen and blood flow to a baby’s brain, causing hypoxic-ischemic encephalopathy (HIE), a leading cause of death or neurological impairment among infants. In the past eight years, cooling therapy (hypothermia) has become the standard form of care for HIE, as it’s been found to […]