When patients and families with sickle cell disease (SCD) call Seattle Children’s to schedule appointments, they are greeted by the friendly voice of Enjoli Harris, who is a skilled member of the SCD patient scheduling team and a “sickle cell mom.” Harris’ youngest child, Nehemiah, was diagnosed with SCD at birth almost 12 years ago […]
For parents with children or teens who are having problems at home or at school for more than six months due to trouble with attention, learning or behavior, understanding if it’s attention deficit hyperactivity disorder (ADHD) or a related disorder, is important. ADHD is a neurodevelopmental disorder and is the most common mental health disorder […]
For American Heart Month, Seattle Children’s providers share their tips for helping kids and teens build strong, healthy hearts. Protect young athletes with pre-sport heart screenings Generally, kids are safe to play sports and exercise without concern for cardiac events, but with all types of sports, it is important to do a physical with family history […]
Throughout this season’s viral surge, Seattle Children’s Urgent Care team has been hard at work caring for a high volume of patients throughout its four locations in Bellevue, Everett, Federal Way and Seattle. The sites are open 7 days a week, including holidays, and recently expanded their reach by offering virtual urgent care services to […]
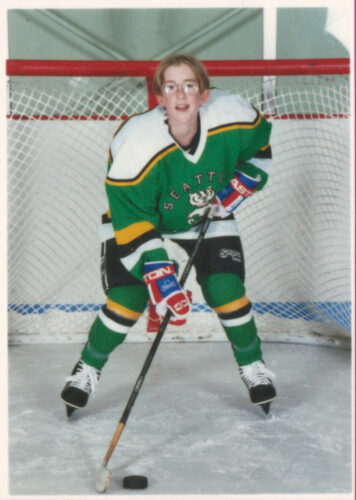
PART FIVE: From witnessing exceptional care and compassion given to children in their own lives, to receiving treatment first-hand, this weekly series features Seattle Children’s employees and the life experiences that drove them to pursue careers in healthcare. During a family vacation in 1993 at Lake Chelan, WA, 12-year-old Jesse Giordano started experiencing severe flu-like […]
Seattle Children’s has teamed up with primary care pediatricians in the Puget Sound region to implement a new approach to address the growing youth mental health crisis. Seattle Children’s Care Network (SCCN) and Seattle Children’s Psychiatry and Behavioral Medicine launched a Pediatric Integrated Behavioral Health Program in 2020 to provide children and their families with […]
On December 12, 2022, Seattle Children’s opened the doors to Seattle Children’s Magnuson, which will serve as the new hub for autism and behavioral health care, outreach, training and research, in order to better meet the needs of youth and families in our community. “Seattle Children’s is working to create a future where every young […]
Pediatric, adolescent, and young adult patients with cancer and blood disorders in the greater Pacific Northwest will be cared for at a new state-of-the-art facility specifically designed for transformative, patient-centered care. On Dec. 5, the Cancer and Blood Disorders Center (CBDC) officially opened the doors to its new outpatient space at Forest B. Forest B […]
Read in Spanish below. Leer en Español más abajo. Carlos Vives, Colombian singer, songwriter and actor, paid a special visit to Seattle Children’s on Tuesday, September 20 to learn about our efforts to provide inclusive care for children and patient families whose first language is Spanish. Vives has been an international figure for decades […]
Seattle Children’s is actively working to identify, validate and innovate how children with pediatric acute and other high-risk leukemias are treated.