Last fall, 20-year-old Milton Wright III was given a death sentence. Today, he is expected to live a long, healthy life. This is the incredible story of how two determined researchers and the parents of a young boy came together to save him. On Sept. 18, 2013, 20-year-old Milton Wright III walked into Seattle Children’s Hospital […]
The heart that connects Rachel Cradduck to a family in Mexico was transplanted into her son Ethan Robbins at Seattle Children’s Hospital when he was just five months old. It came from a baby who died in a California hospital after her family traveled there for medical care. “A heart transplant is a bittersweet thing,” […]
Chrissy Ehlinger had a very normal pregnancy, so when her son Carter was born she had no concerns about his health. He was beautiful and perfect and looked like any healthy baby should. It wasn’t until a simple, inexpensive and non-invasive newborn screening test called pulse oximetry screening revealed the unthinkable. Pulse oximetry testing is […]
Over the past two years, 17-year-old Nicky Richens’ life has transformed. He has found independence and a sense of freedom that he has never before known thanks to a small, discrete device called a phrenic nerve stimulator. Nicky was born with congenital central hypoventilation syndrome (CCHS), a rare disorder that affects the autonomic nervous system […]
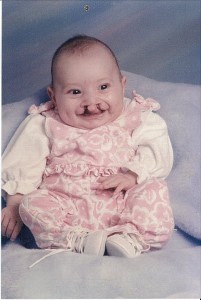
In 2014, the Seattle Children’s Research Institute will implement life-saving projects, begin new studies to keep children safe and continue searching for ways to prevent and cure diseases that threaten some of our youngest patients. We are celebrating the New Year by highlighting some of the work that has researchers excited about 2014. Cleft lip […]
In 2014, the Seattle Children’s Research Institute will implement life-saving projects, begin new studies to keep children safe and continue searching for ways to prevent and cure diseases that threaten some of our youngest patients. We are celebrating the New Year by highlighting some of the work that has researchers excited about 2014. Looking forward […]
At age 4, Natalie Merlo was diagnosed with a facial condition that left her feeling self-conscious and very different from other people. While growing up, she even avoided having her photo taken. Through the work with her care team at Seattle Children’s Craniofacial Center, Natalie has gained confidence, has happily accepted who she is and […]
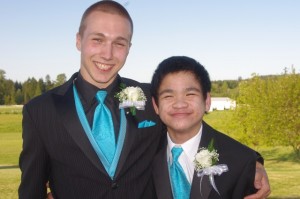
AJ Hwangbo was a happy-go-lucky 6-year-old without a worry in the world until mid-November when he developed a life-threatening heart condition. While specialists at Seattle Children’s Hospital helped AJ heal physically, the young boy struggled to bounce back emotionally. But, AJ’s joyful spirit returned after hospital staff arranged for him to meet his hero – […]
The faster medical research moves the more quickly cures can be found for countless children’s diseases. But one of the greatest delays researchers face when trying to solve medical problems is finding enough patients to study. “Enrolling patients in a clinical trial to study a rare condition could take years,” said Mark Del Beccaro, MD, […]
Being sick is never fun for a child, and spending time in a hospital can be especially difficult for families during the holidays. Children sometimes wonder if Santa will be able to find them come Christmas day. But at Seattle Children’s, there’s no need to worry. Every year, Santa makes a very special visit to […]