
Seattle Children’s has teamed up with primary care pediatricians in the Puget Sound region to implement a new approach to address the growing youth mental health crisis.
Seattle Children’s Care Network (SCCN) and Seattle Children’s Psychiatry and Behavioral Medicine launched a Pediatric Integrated Behavioral Health Program in 2020 to provide children and their families with the mental and behavioral health support they need earlier and closer to home.
The innovative program aims to empower primary care teams to identify, manage and coordinate mental and behavioral health services within their community settings with the long-term goal of alleviating pressure on hospitals and specialty care practices.
“Mental health care is one of the greatest unmet needs in pediatric health, said Dr. Sheryl Morelli, chief medical officer for SCCN. “The support we received from the Seattle Children’s Guild Association’s Funding Hope Award has been instrumental in establishing the foundational components of an integrated behavioral health program across our network, including universal behavioral health screenings and brief evidence-based interventions within primary care.”
Creating a pediatric model
The program helps primary care clinics like Skagit Pediatrics implement standard behavioral health screenings to identify patients and families who need support sooner, offer appropriate, short-term services with a behavioral health specialist at their clinic, and provide a seamless transition to long-term services when needed.
“We wanted to incorporate a more accessible approach to behavioral health care,” explained Dr. Rick Levine, a pediatrician at Skagit Pediatrics.
His clinic, which serves about 10,000 active patients in Mount Vernon, a semi-rural town about 60 miles north of Seattle, was among the first of six primary care practices to participate. Their behavioral health team helps break down common barriers that prevent patients from accessing behavioral health care, including social stigma, limited access and challenges navigating the healthcare system.
The SCCN program team — which includes individuals from clinical, operations and data analytics roles — provides local clinics with implementation and data support, training, education, ongoing coaching, funding, and more to build a sustainable integrated behavioral health model for supporting their community.
Improving access to behavioral health care
Before Skagit Pediatrics hired its first behavioral health specialist, its providers weren’t sure how many of their patients followed through on their referrals and received treatment because they were referring them to other behavioral health resources in the community.
Now, they are equipped to help patients and their families navigate barriers that could prevent them from receiving care, and they have a system to measure their impact. SCCN data analysts help primary care clinics track their health screening rate, the number of referrals to internal and external specialists and the number of visits that result from their referrals. The data provides clinics with critical ongoing feedback to help them evolve to better meet the needs of patients and families.
In the last two years, five of the participating clinics have provided behavioral health services to almost 2,500 patients for a total of 9,200 behavioral health visits.
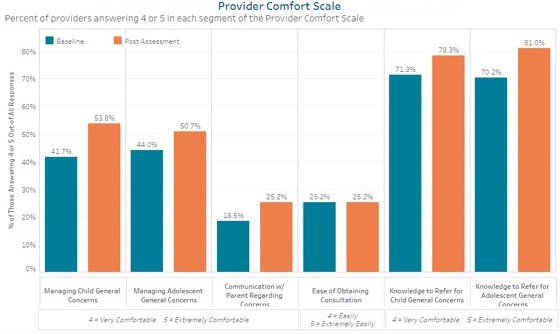
Six additional primary care sites joined the program in 2021. While their patient and visit volume data is not yet available, the SCCN program team has seen provider comfort in managing behavioral health concerns increase in five of the six focus areas across the 12 participating sites. As the program matures, the team hopes to show how its early interventions improve outcomes and reduce the need for higher-intensity mental health services.
About the program
Seattle Children’s Care Network Integrated Behavioral Health Program is part of the national Johns Hopkins Pediatric Integrated Care Collaborative, which promotes integrated healthcare and mental and behavioral health services.
The program also includes components of the University of Washington’s Advancing Integrated Mental Health Solutions Center Collaborative Care Model, an evidence-based treatment approach for common mental health conditions such as depression and anxiety that has led to better patient outcomes, better patient and provider satisfaction, and reductions in health care costs.
The Integrated Behavioral Health Program is part of Seattle Children’s Generation REACH initiative, which aims to reimagine pediatric mental health care so that all children, teens and families can live their healthiest and most fulfilling lives possible.

