HIV is a cunning virus—it infects, takes over and shuts down the body’s T-cells that fight infection. This leaves HIV-positive individuals without immune power to fight off many types of infections, even a common cold, which can become deadly.
Researchers at Seattle Children’s Research Institute published two studies in the journal Molecular Therapy that could lead to a more permanent treatment that uses the power of the immune system to fight off disease. With the use of gene editing, they developed a T-cell that can both kill and resist HIV simultaneously, a promising step forward in the development of HIV immunotherapy.
“Our goal is to develop an HIV treatment that is more permanent than a daily drug,” said Dr. David Rawlings, director of the Center for Immunity and Immunotherapy at Seattle Children’s Research Institute. “In the future we hope this treatment would eliminate the need for HIV drugs that have negative side effects on people who need them to stay alive.”
A shift from drugs to immunotherapy

Modern drugs have allowed HIV-positive people to live longer lives because the drugs suppress the virus. But doctors are still researching an effective long-term solution to HIV because the drugs come with negative short- and long-term side effects, from nausea to more serious conditions like liver complications.
This is especially important research for pediatricians because their young patients have to bear the burden of HIV and its treatment longer than individuals who are infected as adults. Over time people with HIV have higher rates of cardiovascular disease, neurodegenerative problems and cancer, according to Dr. Thor Wagner, an infectious disease specialist at Seattle Children’s Research Institute. These side effects are likely due to the combination of chronic HIV infection and long-term exposure to the antiviral medications.
“Many people don’t realize that HIV is a condition that young people and teens have,” said Wagner. “In fact, about 25% of new HIV infections in the U.S. are in youth ages 13-24, so our patients are in need of better long-term treatments.”
In the recently published studies, Rawlings and Wagner showed that T-cells that have been altered with gene editing could both kill and resist HIV in human blood samples.
“HIV shuts down the tools that a T-cell uses to fight infection, and with this research, we showed that we can reinstall tools for the T-cells to fight back,” Rawlings said. “With gene editing, we gave the T-cell the ability to kill HIV, and we also gave it a ‘shield’ that allows it to resist HIV infection.”
A tricky virus, an iron-clad new T-cell
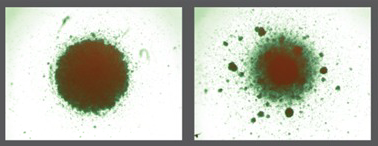
HIV invades T-cells by latching on to different receptors on the cell’s surface, or envelope. These receptors act like locks on a T-cell house, and HIV’s mechanism of entry is to hook into a lock and break into the cell.
The most common receptor HIV targets is called CCR5. Through gene editing, the researchers were able to get rid of this receptor on the T-cells, which makes it much harder for HIV to break into the T cells.

In parallel with getting rid of the receptor, the investigators introduced a chimeric antigen receptor (CAR) into these same T cells. This anti-HIV CAR allows the gene-modified T cell to attack and kill HIV infected cells.
CAR T cells have already been extremely effective in treating leukemia at Seattle Children’s clinical trials including the Pediatric Leukemia Adoptive Therapy (PLAT-02) trial. The researchers are taking advantage of advances in this exciting field to develop a new immunotherapy approach for HIV.
“The exciting achievement in this study is that we were able to package all these capabilities into a single T-cell,” said Rawlings. “Previous clinical trials show that these mechanisms like HIV-killing and HIV resistance work in isolation, but now we’ve created a T-cell that can do all those things at once.
If the research proves to be safe, in the future doctors could extract T-cells from an HIV-positive patient, modify their T-cells, and inject the cells back into the patient where they would kill HIV and resist infection continuously.
A future of improved HIV therapy
The researchers liken this leap to the way current HIV drugs have been combined for easier and more effective therapies.
“Most patients take a single pill each day to keep the HIV under control, but in reality that pill is a combination of several effective drugs,” Wagner said. “We hope this type of T-cell we’ve created would serve the same function someday, and without the ongoing need for drugs.”
The researchers are already testing the safety and effectiveness of the modified T-cells in animal models and hope to develop human trials in the coming years.
“It’s exciting to think that we may be having different conversations with our patients about treatment possibilities in the future,” Wagner said. “They’ve been asking us for better long-term treatment options, and this research takes us in that direction.”
Resources
- Molecular Therapy: Engineering HIV-Resistant, Anti-HIV Chimeric Antigen Receptor T Cells
- Dr. David Rawlings, Seattle Children’s
- Dr. Thor Wagner, Seattle Children’s
- Center for Immunity and Immunotherapies, Seattle Children’s Research Institute

