Arianna Ciccu and her husband, Marco, knew if they had children, they might be born with congenital adrenal hyperplasia (CAH). It’s a genetic condition Marco was born with and has navigated his whole life.
CAH is a group of conditions that affects a person’s adrenal glands. Congenital means the condition is present at birth, and hyperplasia means the glands are overgrown. The adrenal glands make and release the hormone cortisol, which plays a key role in how the body uses sugar for energy and how it deals with stress. A person with CAH can’t make enough cortisol because they are missing an enzyme. There are two different types of CAH, classical and nonclassical. Classical CAH is more severe and can be life-threatening.
When Arianna and her husband welcomed their first child, Rebecca, the first thing they asked the doctor was if Rebecca had CAH. Today, all babies are screened for CAH at birth using a simple blood test. Without treatment, newborns with CAH can develop serious symptoms, including weight loss, vomiting, dehydration, diarrhea, shock, heart rhythm problems and death.
The test was positive.
Finding a second home
The Ciccu family had recently moved to the U.S. from Italy and were learning English when they welcomed Rebecca into the world. Trying to understand a complex medical vocabulary while adjusting to their new roles as parents presented unexpected challenges.
Rebecca was born at the University of Washington Medical Center, and her family was referred to Seattle Children’s for specialized care. Quickly, Seattle Children’s became a second home for the Ciccus. They were there often for blood draws, clinic appointments and follow-up visits. They felt like they had found a place where their child could thrive.
For the Ciccus, Seattle Children’s CAH Center offered hope for a bright future for their daughter and, although they didn’t know it at the time, for their son, Samuele, who would be diagnosed with CAH as well.
“My kids have been diagnosed with CAH since the very first days of their life,” Arianna said. “It has been a roller coaster especially during the first year. We have been involved with every type of care in existence – check-ups, urgent care appointments, emergency visits – but thanks to the prompt services from Seattle Children’s, we have always been able to find a solution and receive the care we needed in a timely fashion.”
Seattle Children’s and the University of Washington formed a multidisciplinary team in 1981 to care for children with differences in sex development (DSDs). Today, Seattle Children’s Differences in Sex Development Program is recognized as a Center of Excellence by the National Institutes of Health. Providers within the DSD Program are all experts in DSDs and provide compassionate, evidence-based care for babies, children and teens with all types of differences in sex development, including CAH.
Seattle Children’s DSD Program is one of the oldest and most established programs in the country and has one of the highest volumes of pediatric patients. It services the largest geographical medical region in the U.S., which covers Washington, Alaska, Montana and Idaho. While CAH is considered a DSD, Seattle Children’s treats patients with CAH in a separate program focused exclusively on CAH.
“Patients with CAH have unique problems, so we decided to create a CAH program specifically to meet their needs,” said Dr. Patricia Fechner, Medical Director of Seattle Children’s CAH Center.
Seattle Children’s is designated a CAH Center of Excellence and a Level 1 Comprehensive Care Center for CAH by the CARES Foundation.
Around the time of Rebecca’s first birthday, she needed to undergo surgery. Fechner sent her to see Dr. Margarett Shnorhavorian and Dr. Mark Cain, surgical co-directors of the CAH Center. They are internationally recognized experts in surgical care for children with CAH and other DSD conditions.
Finding a home
Fechner came to Seattle Children’s about 15 years ago to help build the DSD Program. From her budding years as a medical student, she knew she wanted to be an endocrinologist. She loved engineering and medicine, and endocrinology provided the perfect junction of her interests. After her residency, she completed a fellowship at Johns Hopkins University School of Medicine, where she was at the forefront of DSD and CAH care and research.
Her vision for the program at Seattle Children’s was to make coordinated, comprehensive care easy for patients and families. Children with DSDs require care from a team of specialists, including experts in endocrinology, genetics, urology, gynecology, pediatric surgery, child and adolescent psychology and more.
“What makes us truly unique is the way in which we see patients and families,” Fechner said. “All of the specialists meet simultaneously with the family as a team. We are supportive of each other and work very well as a team. We are all experts in our field but together as a team, we are even stronger. Our infrastructure is set up to help families. Instead of asking a family to repeat their history over and over again, they only have to do it once. We all hear the same thing and can make a cohesive plan together. We are so happy to be able to offer a separate but parallel program for our patients with CAH and are very proud to have received the prestigious designation as a CAH Center of Excellence and a Level 1 Comprehensive Care Center for CAH.”
“Dr. Fechner is like a family member for us and has always been supportive throughout the years,” Arianna said.
Research advancements to help patient thrive

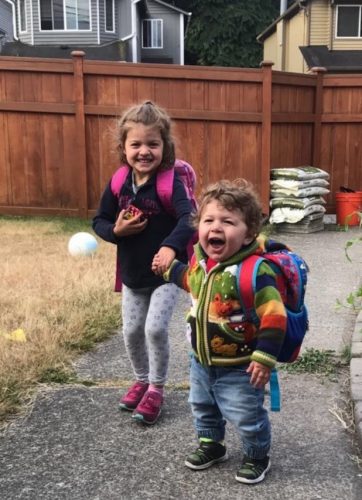
Today, Rebecca, 9, and Samuele, 6, see providers within the CAH Center of Excellence every few months.
For the rest of their lives, they will be on medication to manage the health effects of CAH. You would never know by looking at them. They are both healthy and active and enjoy playing soccer.
Their family has been involved in research to find better medications to manage CAH.
“For the last 45 years, we’ve only had a handful of medications, but today, studies are looking at new methods for treating congenital adrenal hyperplasia,” Fechner said. “The goal is to hopefully decrease the amount of hydrocortisone or glucocorticoid that a patient needs and thus the amount of side effects they face in adulthood.”
Marco was excited to participate in a trial when presented with the opportunity.
“My children will live with CAH for the rest of their lives, but I hope science can help,” Arianna added. “There’s been a huge difference from when my husband was born until now. He wanted to be involved in research to help move innovation forward. He wanted to do it for our kids.”
Fechner says the aim of the CAH Center is simple.
“We want every child to have the best life possible,” Fechner said. “Watching these children grow has been rewarding. For more than three decades, it’s been an amazing experience.”

