 Eighteen months ago, Dr. Lynn Martin, an anesthesiologist and medical director of the ambulatory surgery center at Seattle Children’s, and his colleagues at the Seattle Children’s Bellevue Clinic and Surgery Center set out to reduce the use of opioids during outpatient pediatric surgeries, while maintaining or improving pain management and outcomes for patients. Ultimately, they accomplished much more by successfully ousting opioid use during surgeries.
Eighteen months ago, Dr. Lynn Martin, an anesthesiologist and medical director of the ambulatory surgery center at Seattle Children’s, and his colleagues at the Seattle Children’s Bellevue Clinic and Surgery Center set out to reduce the use of opioids during outpatient pediatric surgeries, while maintaining or improving pain management and outcomes for patients. Ultimately, they accomplished much more by successfully ousting opioid use during surgeries.
According to the Centers for Disease Control and Prevention (CDC), drug overdose deaths continue to increase in the U.S. It is a problem Martin and his colleagues believe they can help address, which is what drove them to develop a novel initiative at Seattle Children’s to reduce opioids.
Martin and his colleagues completed their breakthrough quality improvement initiative to reduce opioid use and their findings were published in Anesthesia and Analgesia.
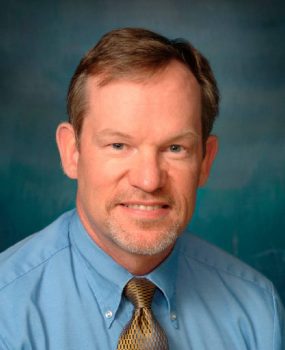
Here’s more from Martin about their initiative in a Q&A:
Q: What compelled you to reduce the use of opioids?
A: We are living in an opioid epidemic. According to the CDC, two out of three drug overdose deaths involve opioids and more than 130 Americans die every day from opioid overdose. Often in medicine, a simple surgery can be the introduction of an opioid to a patient, thus opening the door for addiction. As a physician I feel somewhat responsible. This non-opioid breakthrough can potentially prevent addiction by never exposing patients to the drug in the first place.
Q: How did this quality improvement come about?
A: Although we always planned to use as little opioid as possible by using combinations of medicines for pain relief, no one thought total elimination of opioid use was possible. We never set out to oust opioids, but in January of 2019, after it worked so well for our top 12 surgeries, we decided to remove the opioids, morphine or fentanyl in most cases, from all procedures.
We initially began working to develop an effective non-opioid anesthesia plan by looking at tonsillectomies, or the removal of the tonsils, because it was one of the most common procedures and was also known to be painful. Anesthesiologists safely combine medications to manage pain and sedation, which typically includes an opioid and a form of acetaminophen in the intravenous therapy (IV). The IV acetaminophen is very expensive, so my initial proposal to the team was to find an alternate for it. The first iteration cut the opioid in half and combined it with dexmedetomidine, a drug used for sedation that also provides some pain relief. Later we removed the opioid altogether and substituted ketorolac, a nonsteroidal anti-inflammatory medicine, to be used along with the dexmedetomidine. Ultimately, we have learned that this combination works not just on tonsil surgery, but on all outpatient surgeries.
Since starting this initiative, more than 6,000 patients have undergone surgery without opioids during their procedure. Technological tools provided access to the data we needed that allowed us to learn, improve, and rapidly spread our new practices.
Q: How does this new combination medicine work and is it as effective as opioids?
A: In our quality improvement initiative, we found we were able to safely anesthetize patients, manage pain after surgery, eliminate nausea after the surgery (as the opioid was causing it) and theoretically reduce the risk for post-op addiction without the use of opioids and without compromising patient outcomes. The fact that this alternate combination of medications is less costly was just bonus.
Q: Anecdotally, what has the parent response been to this change?
A: Understandably, parents are concerned about opioid use given the education and media coverage that has emerged over the past few years. They have been pleasantly surprised and appreciative to learn the Seattle Children’s Bellevue Clinic and Surgical Center no longer uses opioids during surgery.
Parents have also appreciated learning that the Pain Management team at Seattle Children’s has more than 10 years of history working to provide safe relief of acute and chronic pain. Many of these efforts are designed to reduce the use of opioids through methods such as biofeedback, visualization, and acupuncture among others.
Q: Can parents request non-opioid surgery?
A: I encourage parents to discuss the anesthesia plan and their preferences with their child’s anesthesia provider(s) who will do their best to come up with a mutually acceptable plan. Parents should also ask questions about how their child’s pain will be treated after surgery and if opioids can be avoided. Non-opioid pain treatment options (ibuprofen, acetaminophen) should always be used first for pain and opioids used only if the child is still experiencing pain.
While anesthesiology has been spearheading our efforts to reduce opioid use at Seattle Children’s, all surgeons and other physicians who prescribe medicine also have stepped up their efforts to do their part to reduce the opioid epidemic. As a general rule, surgeons make every effort to reduce the use of opioids for pain treatment following surgery. However, if the patient will need opioids after surgery, parents should store the medicine safely in the home during recovery and manage dosages for their child. It is important parents are prepared to safely dispose of any unused medicines after their child has recovered. Removing unused prescription medicine from the home can help prevent the risk of improper use and the potential for addiction.
The Washington State Healthcare Authority recently launched a campaign to educate adults and parents about opioids in the hopes of curbing the opioid epidemic by safely disposing of prescription opioids to prevent misuse. This link provides locations throughout the state of Washington to turn in unused medicines.
Parents should also discuss with their surgeon where the procedure will be scheduled. Surgeries within the Seattle Children’s system are only performed in two locations. Smaller, less complex cases are typically scheduled in the Seattle Children’s Bellevue Clinic and Surgery Center while bigger, more complex operations that require a hospital stay of a night or more are scheduled for Seattle Children’s main hospital.
Q: How is this progress personally rewarding to you?
A: This continuous improvement process has kept me going in my career. While I was contemplating retirement, I started to see things happening that I never thought would happen. It made me want to explore and share these opportunities with my colleagues in Seattle and elsewhere. I’ve been in medicine for 30 plus years and in my career, I’ve tried to make life better for my patients and their families. Now I can do this on a much bigger scale.
Q: What’s next? How does this advance healthcare into the future?
A: I see several next steps. First, we need to continue working with our surgical colleagues to reduce or eliminate the need for opioids after surgeries when patients go home. Next, we need to start thinking about how we can apply this practice to more complicated and more painful surgeries that typically require a hospital stay. And finally, we need to explore if this can be applied not only to pediatric patients but to adult patients as well.
We have already started sharing our positive results via presentations at regional and national meetings as well as publication in journals. In addition, we have done some limited work for children with more complex surgeries that require hospital admission with early positive results at our main campus in Seattle. We are working to expand this practice within Seattle and are eager to spread it to the Washington, Alaska, Montana, Idaho (WAMI) region and beyond.
Resources
- Anesthesia Basics
- In Pursuit of an Opioid-Free Pediatric Ambulatory Surgery Ce… : Anesthesia & Analgesia (lww.com)
- Bellevue Clinic and Surgery Center (seattlechildrens.org)
- Take Back Your Meds – Take Back Your Meds

