In 2019, Samantha and Kyle Hatch received wonderful news: Samantha was pregnant with identical twins. The couple already had two kids, Ben and Penny, and envisioned all of the roughhousing, road trips and happy mayhem that comes with four children. But everything changed when a routine ultrasound showed that one of the twins, William, had […]
On the Pulse
Seattle Children’s providers, nurses and other team members chose their professions because they care deeply about helping kids live the healthiest and most fulfilling lives possible. For them, it isn’t about winning awards — it’s about the positive impact they can have on patients’ lives. But by performing their jobs in an exemplary fashion, they […]
Dr. Molly Taylor recently found a long-forgotten journal from her college years. In it, she asked her young adult self: “Do I want to be a pediatric oncologist?” It turns out she did, and she went to medical school after studying psychology and microbiology as an undergrad. Bringing together of all those disciplines, today she’s […]
Before she was diagnosed with high-risk acute lymphoblastic lymphoma (ALL), Kinsey was an active 15-year-old who enjoyed competitive horseback riding, spending time with her family and friends, and dreaming about what her future might look like. Less than two months into her cancer treatment at Seattle Children’s, however, Kinsey became a shell of herself. While […]
In a major moment for combatting respiratory syncytial virus (RSV), on Sept. 22 the Centers for Disease Control (CDC) recommended an RSV vaccine for pregnant persons that researchers have determined is safe and effective in preventing RSV disease in infants through immunization during pregnancy. The new Pfizer RSV vaccine joins the recently approved monoclonal antibody, […]
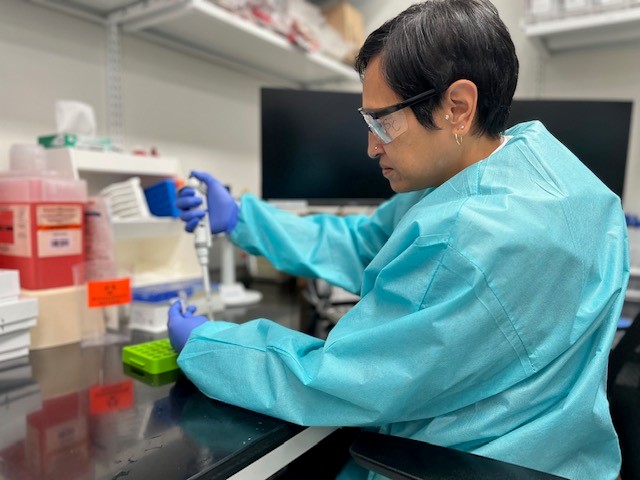
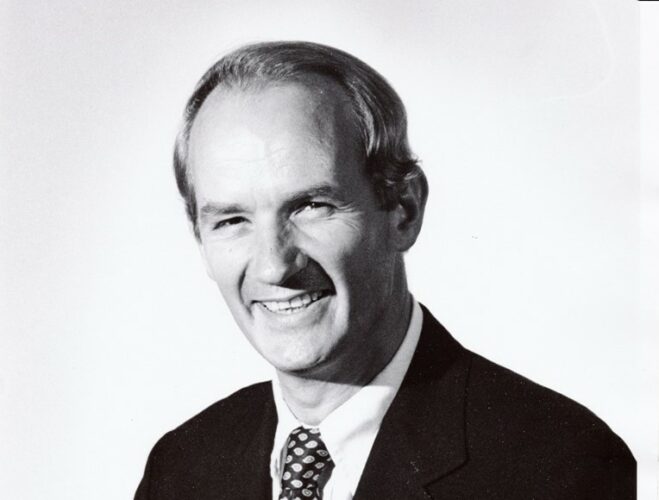
In honor of the late Dr. Peter Mansfield, former Seattle Children’s Chief of Surgery, his wife, Jackie Mansfield, has established a fund directly benefitting the Invent at Seattle Children’s Postdoctoral Scholars Program (Invent@SC), which is an investment in training for early career scientists historically underrepresented in or excluded from biotech in the development of therapeutics for childhood […]
Seattle Children’s has appointed Dr. Vittorio Gallo as senior vice president and chief scientific officer. As senior vice president and chief scientific officer, Dr. Gallo will serve as the principal scientific executive of the health system and partner with Chief Research Operations Officer Dr. Eric Tham and Chief Academic Officer Dr. Leslie Walker-Harding to provide […]
It’s estimated nearly 86,000 adolescents and young adults (AYAs) will be diagnosed with cancer this year; in fact, one-third of patients treated for cancer at Seattle Children’s are AYAs. These 15- to 39-year-olds face the unique challenges of their life stage — finishing high school or college, starting a career, establishing independence, finding a romantic […]
On Sept.12, leaders from Odessa Brown Children’s Clinic (OBCC) announced the location of its new clinic site in Seattle’s Central District. The future home of OBCC, situated on the corner of 18th Ave. S. and S. Jackson St., will serve area patients and families with robust mental health and behavioral health services, nutrition, acute and […]
As a second-year grad student working toward a doctorate degree in the field of health sciences, Emma is as busy as ever. But for this 23-year-old, originally of Snohomish, WA, facing extraordinary challenges with determination and resilience is a skill she mastered early on. In 2017, after experiencing extreme bouts of itchiness from head to […]