Dr. Katie Williams, a pediatrician and urgent care specialist at Seattle Children’s Bellevue Clinic and Surgery Center, lived every parent’s worst nightmare when her 1-month-old son turned gravely ill one Saturday evening in January. Here, Williams shares how her infant escaped the grip of death — and how she gained a new level of gratitude — thanks to her colleagues’ expertise in pediatric life support.

The Saturday that is forever burned in my memory started out typically. My husband David DeTerra and I took our three kids — 4-year-old Evan and 1-month-old twins Elisabeth and Grayson — to an afternoon birthday party for a friend. On the way home, we stopped for takeout and looked forward to a relaxing evening at home. I remember sitting in the car thinking how glad I was that the twins had reached the 30-day mark, because that’s the point where infants are less likely to get serious infections.
What happened next came totally out of the blue.
Grayson started breathing funny and he had this strange rhythmic cry. I figured he was hungry and wanted out of his car seat to nurse. When we got home, David noticed he felt cool and clammy and his face looked pale. We both tried to feed him, but he wouldn’t eat. His eyes, normally so alert, couldn’t connect with us at all. When his tiny body went limp, we frantically called 9-1-1.
The ambulance came and the team tried to take us to the community hospital that’s five minutes from our house, but I pushed back because emergency room physicians at community hospitals tend to treat more adults than children. They do pick up some pediatric training, but medical care for very critically ill infants is incredibly specialized these days. Instead, I insisted they make the 40-minute drive to Seattle Children’s Hospital. In hindsight, that was the best decision I’ve ever made.
Ready for any medical crisis
When we got to the emergency room (ER), we were greeted by attending physician Dr. Eileen Klein while a team readied to treat our son in the large resuscitation room. (Later, I learned that the ER team built a full- scale cardboard mockup of their resuscitation room in a warehouse in order to test that the design could handle absolutely any medical crisis.)
Dr. Klein immediately comforted us and included us in Grayson’s assessment, even asking if there were other lab tests that I thought he needed. We never felt like bystanders, which is the team’s goal with every family: we felt empowered and our involvement gave us something to focus on besides the fear that our son might not survive.
At first, Grayson seemed to bounce back. I started to feel a little embarrassed, like we’d overreacted. All of a sudden I heard a nurse yell, “he’s crashing,” and we watched a monitor show his heart rate drop dangerously low.
I remember Evan asking, “Will Grayson die?” That’s when the ER social workers stepped in and took Evan and Grayson’s twin, Elisabeth, to a room away from the busy scariness, fed them and distracted Evan with a movie. I am forever grateful that they were so protective of our family at that very vulnerable time. I can’t thank them enough for making sure our preschooler didn’t witness the intensity that followed.
Leaning on life support

For 48 terrifying minutes, the team used CPR and medication to keep Grayson alive. He was close to flat-lining…his pulse was so faint. As I braced myself in the doorway of the resuscitation room and David sat slumped on the floor — both of us in shock — Dr. Carmen Coombs, an emergency medicine specialist, stayed by our side and talked us through every step of what was happening and answered all of our questions. She even called our parents, since we were in no shape to talk with them. Throughout the ordeal, Dr. Klein continued to check in with us. I dreaded she might recommend we stop CPR and let our son go.
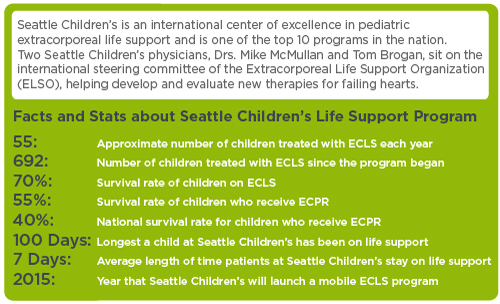
But Dr. Klein never gave up even when it was clear Grayson wasn’t improving. Instead, the team made the call to put him on an extracorporeal life support (ECLS) machine, or ECMO, that would take over the work of his heart and lungs. While ER clinicians kept our boy alive with CPR, surgeons worked in concert with them to hook him up to the life support system — a process known as ECPR. This was only the second time that Seattle Children’s doctors performed the delicate procedure to put a child on life support in the ER – something that’s almost never done outside of an operating room or intensive care unit and has probably never been attempted by any other hospital in our region.
Once Grayson was stabilized, we started the journey to move him from the ER to the Pediatric Intensive Care Unit (PICU). The clinicians stretched out into a long line that moved very slowly; it felt like a funeral procession, even though our baby was alive. We were so scared. That night, in a daze, I sent the following Facebook post to our friends and relatives:
Jan. 18, 2014
Please pray for our son Grayson. He became lethargic and went into cardiac arrest tonight. We are at Children’s PICU and he is on heavy life support. He needs all the positive thoughts he can get. Forgive us for being out of touch in the coming weeks. We will update as we can.
Though the life support system was saving our son, it also put him at risk for complications, including internal bleeding and infections. The entire five days Grayson was on the ECLS machine, two nurses were in Grayson’s room round the clock to ensure his health and safety. I didn’t know much about ECLS before and I was surprised — and so very grateful — for the intense monitoring.
Jan. 21, 2014
Grayson had another good night. He was able to open his eyes and I cried from happiness to see him looking at us again. There are so many people at the hospital watching out for him. He (and we) are in good hands.
The road to recovery

We spent 11 days in the PICU and the doctors and nurses made us feel like we were the only family there. Through all the emotional ups and downs, they were by our side. Dr. Reid Farris, Grayson’s lead physician, would come to our room to sit and talk with us after he finished his rounds — a daily occurrence that never felt rushed. (Even after Grayson was transferred to the general medical floor, members of the PICU team continued to visit us on their lunch breaks!)
And it wasn’t just my husband and I who received such compassionate care. Child life specialists gave Evan a medical kit so he could practice putting medicines and tubes into a special doll. He got so comfortable with all the medical supplies that when my dad finally brought him to visit Grayson, he gave his little brother a kiss and said, “Can I go play now?” (Evan thought the hospital was a fun hotel where he could visit the Playroom and Therapy Pool and watch the helicopters land outside Grayson’s window.)
In total, we lived at the hospital for a month. Though many doctors tried to crack Grayson’s diagnosis — including me — no one has yet to figure out why he got so sick. We had a running joke that everybody but Adolescent Medicine tried to solve Grayson’s puzzling case.
 Grayson and Elisabeth are now 11 months old and he’s as sweet, social and smiley as she is spirited. Though he’s a bit behind his sister in gross motor skills — and still sees doctors in a number of Seattle Children’s clinics including cardiology, neurology and urology — our little fighter is making his way back to peak health. We also remain connected to some of the team who cared for Grayson in his darkest hour — a testament to the love and compassion that is at the very foundation of this amazing hospital.
Grayson and Elisabeth are now 11 months old and he’s as sweet, social and smiley as she is spirited. Though he’s a bit behind his sister in gross motor skills — and still sees doctors in a number of Seattle Children’s clinics including cardiology, neurology and urology — our little fighter is making his way back to peak health. We also remain connected to some of the team who cared for Grayson in his darkest hour — a testament to the love and compassion that is at the very foundation of this amazing hospital.
As for me, I grew up in Renton, Wash., and attended the UW School of Medicine. I completed my medical residency in Milwaukee, but I always hoped to do my life’s work at Seattle Children’s. What I didn’t know was that our son would end up owing his life to the hospital. Sometimes I work a shift in the ER and every time I walk past that resuscitation room, I think about the night Grayson crashed. Every time, I am grateful for my son and Seattle Children’s.
Donate now to Seattle Children’s Greatest Needs and help patients like Grayson receive the most advanced lifesaving care in our region.
Resources
- Seattle Children’s Heart Center
- Seattle Children’s Emergency Department

