
In February, Madison Fairchild, 7, waited patiently with her family in a pre-op exam room at Seattle Children’s Hospital.
As they waited for Madison to be taken into surgery she asked one question: “Are they going to take all the bad things out?”
The simple answer was yes, thanks to a new procedure pioneered at Seattle Children’s that uses a common household item to remove tumor-like growths called venous malformations: super glue.
That’s right, super glue.
Seattle Children’s is currently one of only two centers in the country to offer the new, revolutionary procedure.
A new procedure, a new hope
Madison was born with a venous malformation on her thigh and calf. The tangled cluster of extra veins caused her extreme pain and limited her ability to walk. Growing up, she typically stood balanced on one leg, with the other bent at a 90-degree angle. When she did walk, she did so with care.
“She was our little flamingo,” said Kristen Fairchild, Madison’s mom.
Madison and her family were hopeful their journey to remove the malformations from their daughter’s leg was finally coming to an end. They were excited for the pain to be gone and for Madison to be able to walk normally again.
Madison underwent a procedure called glue embolization where medical-grade glue is injected into venous malformations. Once the glue hardens, surgeons are able to easily remove the extra veins.
Glue embolization was first developed at Seattle Children’s to remove venous malformations in the head and neck, but the technique has been expanded to now treat children with malformations in extremities.
Out of options
Venous malformations are common, and while they vary in severity, can be painful and debilitating in children, limiting their ability to walk or do the fun activities children ought to be enjoying. They are present at birth and grow with a child. Though the bundled veins are filled with blood, they’re not used by the body. They are often, though not always, visible on the outside as a purple mass.
“They can be small and not cause any problems, or they can be quite extensive, encompassing almost the entire leg or arm,” said Dr. Giridhar Shivaram, a Seattle Children’s interventional radiologist.

Dr. Antoinette Lindberg, a Seattle Children’s surgeon, added, “By the time these children see us, they’re often taking over-the-counter pain medications and many have cut back on activities. Sometimes just walking around school is a challenge, and they’re not able to keep up with peers.”
Madison’s malformation was diagnosed at age 3, when the pain started.
“We would just barely brush her leg, and it hurt,” said Fairchild.
At the time, the best treatment available for Madison was sclerotherapy, a procedure where detergent is injected into the malformation to chemically injure the lining of the veins and make them shrink.
“We tried sclerotherapy three times,” said Fairchild. “We were trying to give her some pain relief, but each time it only worked for a couple weeks.”
Fairchild and her husband, JJ, were told there were no other treatment options, so they took a break from sclerotherapy.
“There are cases where sclerotherapy works really well,” said Shivaram. “But it causes a lot of pain and you can never get rid of the entire malformation. And in some cases, like Madison’s, their pain actually gets worse after sclerotherapy.”
The other typical treatment for venous malformations is surgery, but the slippery veins are difficult to remove. Lindberg likens pulling out the veins to tugging on wet tissue paper. And to make matters worse, the veins bleed, which can lead to a blood transfusion.
At the same time Madison took a break from treatment, Shivaram, Lindberg and interventional radiologist Dr. Eric Monroe started experimenting with using glue embolization on legs and arms.
In September 2015, Madison underwent her first glue embolization procedure. Her malformation ran from her hamstring, behind her knee and into her calf. The first procedure focused only on the hamstring portion, which was causing Madison the most pain.
The procedure worked. Like a switch, the pain in her hamstring was gone and her walking dramatically improved.
But she was not yet out of the woods. Over time, the remaining malformation in her calf started bothering her. Madison’s family and her care team decided it was time for another — hopefully final — surgery, which would remove the rest of her malformation and lengthen her hamstring.
Taking out the bad things
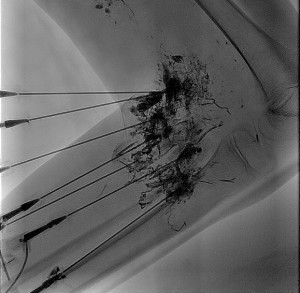
Under anesthesia, Madison was sent to radiology where she was surrounded by ultrasounds, X-rays, CT scans and MRIs. Through real-time imaging, Monroe was able to see his needle enter Madison’s leg as he injected the medical-grade super glue into only the veins he wanted to remove.
After he finished with the glue, Monroe used a low-dose CT scan to make a 3-D image of the malformation, which was then sent to the surgeons as Madison was rolled down the hall, still under anesthesia, to the operating room.
In the operating room, surgeon Lindberg removed the glue-hardened malformation.
By the end of the procedure, all the bad things were finally gone, just as Madison hoped they would be.
New standard of care
Seattle Children’s has performed 50 glue embolization procedures since they started using it 18 months ago. It’s been so successful compared to other treatment options that it has become the new standard of care for venous malformations.
“We want to get the word out about this because it is so effective,” says Shivaram. “There are thousands of children who are not getting optimal therapy for this, and you can’t get this procedure at other places.”
Helping others walk again
Unfortunately, Madison’s case isn’t rare. Thousands of children and adolescents across the U.S. suffer from venous malformations and live with debilitating pain.

When Avery Strozyk,15, was first diagnosed with a venous malformation on her foot at age 12, the pain she lived with on a daily basis was excruciating. The once active teenager was sidelined from sports. But the toll from the malformation took more from her than just the sports she loved; it affected her psychologically as well.
“I had to give up a lot,” said Strozyk. “Every time I’d try to run, my foot would say no. It was too painful. Giving up sports was the toughest thing I’ve ever had to do.”
Like Madison, Strozyk underwent two ineffective sclerotherapy treatments. She was at what would have been the end of the road at other hospitals. Glue embolization offered her new hope and the possibility to get back to the sports she loves.
“If she had been treated anywhere else, there would have been no other option,” said Lindberg.
Three days after the glue embolization procedure at Seattle Children’s, Strozyk was able to walk again without the assistance of crutches. Within a few months she was back in the game.
“I’m happy to be back doing the things I love,” said Strozyk. “Doctors at Seattle Children’s changed my life. They are truly my heroes and I can’t thank them enough.”
Families who want more information or wish to make an appointment can email the Vascular Anomalies care team here: [email protected].

