 You may have heard about a respiratory infection that hit babies and young children particularly hard last year, sometimes resulting in hospital stays. The infection was RSV, which is short for respiratory syncytial virus.
You may have heard about a respiratory infection that hit babies and young children particularly hard last year, sometimes resulting in hospital stays. The infection was RSV, which is short for respiratory syncytial virus.
As RSV season arrives this year, Dr. Tony Woodward, medical director of emergency medicine at Seattle Children’s, shares information to help parents and caregivers keep their families as healthy as possible through this viral season which also includes flu and COVID-19.
There is an exciting new development in the efforts to minimize the impact of RSV for our vulnerable infants. Read on to learn more.
What is RSV?
RSV is a virus passed from person to person that affects the nose, throat and lungs. People of any age can get RSV, but it’s most serious for young children and older adults. Most kids are infected with RSV at least once before they’re 2 years old. For healthy people, RSV usually results in a cold, but some people get very sick, developing bronchiolitis, wheezing/asthma or pneumonia.
Bronchiolitis due to RSV is the leading cause of hospitalization for infants in the United States, but according to the American Academy of Pediatrics, only about 3% of children with RSV will require a hospital stay.
RSV season typically runs from December to April, with a peak of infections in February and March, but last year we saw an early and severe RSV season. Hospitals around the country, especially children’s hospitals, saw unusually high numbers of RSV cases, putting additional strain on the already-stretched healthcare system.
While not all patients who test positive for RSV require the supportive care provided during a hospital stay, some need to be admitted to receive aggressive suctioning to remove secretions, oxygen to help with breathing difficulties and/or hydration through an IV. Last year, those children were arriving at hospitals that were often already full and often over capacity.
“The Seattle Children’s Emergency Department (ED) saw record high numbers of pediatric patients last fall,” said Woodward.
What are the symptoms of mild RSV?
Concerning symptoms include faster breathing, evidence of increased work of breathing/respiratory effort (retractions) and lower levels of oxygen (cyanosis, or blueness). Additional RSV symptoms can include low grade fever, cough, runny nose or congestion, sneezing, poor feeding and fussiness.
There’s no specific treatment medicine for RSV, but you can treat the symptoms if your child is uncomfortable. Fever medicine and fluids can help with symptoms. (Note that babies often do better with more frequent, lower volume of fluids, to allow them to catch their breath while eating.) Acute symptoms usually last 5 to 7 days, but the residual respiratory symptoms can last for weeks. See the resources below for how to treat mild symptoms.
What are the symptoms of RSV that need medical attention right away?
Call your child’s regular healthcare provider right away if your baby or child:
- Is less than 8 weeks old and has a fever (body temperature over 100.4 degrees F).
- Has sustained fever over 104 degrees F, no matter their age.
- Is lethargic or hard to arouse.
- Is experiencing trouble breathing (fast or harder).
- Is dehydrated (no tears when crying, no (or dark) urine in 8 to 12 hours or very dry mouth).
- Has RSV symptoms along with a chronic health condition, like a heart defect or lung disease.
You know your child best, so please contact your healthcare provider if you’re concerned. Use telehealth or urgent care if your child’s provider’s office is closed.
When RSV is severe, your baby or child may have trouble breathing, called respiratory distress. Signs can include:
- Fast breathing
- Flaring nostrils
- Drawing in of chest between, over or under ribs during breathing
- Wheezing when breathing in or out
- Grunting (making noises when breathing out)
- Changes (bluish) in skin color around the lips and under eyes. (This may not be as visible on darker skin tones.)
Pay close attention to your child’s breathing and behavior. If your child is having severe difficulty breathing, call 911.
Which babies and young children are most at risk of severe illness from RSV?
Some babies and young children have a higher risk of a severe RSV infection. They include:
- Babies who are 12 weeks old or younger when RSV season begins.
- Premature babies (especially those born before 29 weeks gestation).
- Babies born with low birth weight.
- Children with chronic lung disease, certain heart defects or weak immune systems due to illness or treatments.
- Children exposed to secondhand smoke at home or whose mother’s smoked during pregnancy.
How can my family avoid getting RSV?
Dr. Woodward offered these tips to help protect your family from RSV and other viruses:
- Limit exposures.
- Stay home from daycare, school and work when sick.
- Ask family and friends not to visit your home or attend gatherings when they’re sick.
- Consider wearing a mask when in public or around those you don’t live with.
- Wash hands often and well. Teach your child how to wash properly.
- Use hand sanitizers often.
- Cover noses and mouths when coughing or sneezing.
- Use tissues or the crook of your elbow when you cough or sneeze.
- Throw tissues away in a covered trash bin right after use.
- Keep your hands away from your face.
- Avoid sharing personal items, such as binkies, utensils, toothbrushes, towels and toys.
- Clean surfaces often, including toys, doorknobs, phones and keyboards.
Is there a vaccine to protect against RSV?
There is a new RSV vaccine, approved with the help of research from Seattle Children’s, that is given to pregnant people. It helps protect babies from birth to 6 months. People pregnant during RSV season can get the vaccine when they are between 32 and 36 months pregnant.
There is an immunization for infants under 8 months who are born during or entering their first RSV season. The immunization is also helpful for some older babies who are at high risk for severe RSV illness and are entering their second RSV season. This should be available through your primary care provider.
In some cases, doctors prescribe a series of monoclonal antibody shots for infants who are at very high-risk of severe RSV infection. Your baby’s doctor will discuss this with you if they recommend this treatment to help prevent RSV in your high-risk infant.
There is also an RSV vaccine for people 60 and older.
Vaccines and other treatments can be a bit confusing, so be sure to ask your doctor or your child’s doctor if you have questions.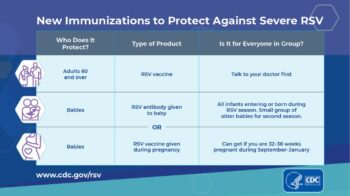
Resources:
- RSV-Bronchiolitis
- RSV: When It’s More Than Just a Cold
- Colds
- How to Suction Your Baby’s Nose (PDF)
- Fever (0 to 12 Months)
- Fever
- Breathing Trouble
- Emergency or Urgent Care?
- Seattle Children’s Urgent Care Clinic in Seattle
- Seattle Children’s Urgent Care Clinic in Bellevue
- Seattle Children’s Urgent Care Clinic in Everett
- Seattle Children’s Urgent Care Clinic in Federal Way

