Kind and sassy Olive Ray is a typical fifth grader, with a deep love for Taylor Swift, horses, chocolate ice cream, and her little sister, January. But the 10-year-old also has some special skills, like having fun even while getting chemotherapy, raising thousands of dollars for brain tumor research and explaining how clinical trials work […]
Over the past 18 months, members of the Seattle Children’s Sickle Cell Disease Program has continued working diligently to improve and enhance care for children, teens and young adults with sickle cell disease (SCD) by expanding services, hours, and staffing, with a special focus on hiring a diverse team that represents the nearly 150 patients […]
In August 2020, just after her third birthday, Aisley began to experience concerning symptoms: headaches in the back of her head, a lack of appetite and vomiting. After a visit to her pediatrician, Aisley was sent to Seattle Children’s for an urgent neurology visit, where she passed the exam with “flying colors,” showing no signs of trouble. Still, Dr. […]
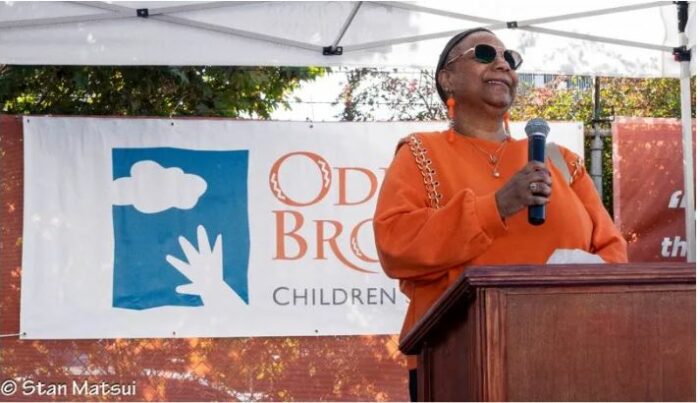
Hundreds gathered in Seattle’s Central District neighborhood to celebrate the Odessa Brown Children’s Clinic’s (OBCC) future location on 18th Ave. S. and S. Jackson St. at a community homecoming event to learn about the services that will be provided, meet their neighbors, enjoy food from local vendors and celebrate the day with family-fun activities.
During a regular 12-week prenatal visit, Mollee Lewallen’s obstetrics appointment went from routine to worrying in a matter of seconds. “We found out that our son, Knox, had an extremely high heart rate,” she explained. “After that appointment, we went to a follow up where his high heart rates continued, so we were recommended to […]
Stage was born three weeks premature and soon began having seizures. He was diagnosed with mitochondrial myopathy, a life-threatening diagnosis with no cure and which causes significant muscular and neurological problems. For Stage and his family, it meant unexpected, lifelong care. “I was naïve enough to think that insurance covered everything if your kid was […]
In 2019, Samantha and Kyle Hatch received wonderful news: Samantha was pregnant with identical twins. The couple already had two kids, Ben and Penny, and envisioned all of the roughhousing, road trips and happy mayhem that comes with four children. But everything changed when a routine ultrasound showed that one of the twins, William, had […]
Seattle Children’s providers, nurses and other team members chose their professions because they care deeply about helping kids live the healthiest and most fulfilling lives possible. For them, it isn’t about winning awards — it’s about the positive impact they can have on patients’ lives. But by performing their jobs in an exemplary fashion, they […]
Before she was diagnosed with high-risk acute lymphoblastic lymphoma (ALL), Kinsey was an active 15-year-old who enjoyed competitive horseback riding, spending time with her family and friends, and dreaming about what her future might look like. Less than two months into her cancer treatment at Seattle Children’s, however, Kinsey became a shell of herself. While […]
In a major moment for combatting respiratory syncytial virus (RSV), on Sept. 22 the Centers for Disease Control (CDC) recommended an RSV vaccine for pregnant persons that researchers have determined is safe and effective in preventing RSV disease in infants through immunization during pregnancy. The new Pfizer RSV vaccine joins the recently approved monoclonal antibody, […]