Seattle Children’s patients were surprised by a special visit by actor Rainn Wilson, known by many as Dwight from comedy series, “The Office.” Patients, families and staff joined in on the fun with viewing parties held both in their hospital rooms and in-person at the main campus. Seattle Children’s Child Life team members emceed the […]
On the Pulse
Laura Licea joined Seattle Children’s in July 2023 as vice president (VP) of Perioperative and Procedural Services and associate chief nursing officer. She brings a fresh perspective and an extensive background in the operating room (OR) from her previous roles at organizations such as UCSF Benioff Children’s Hospitals. Licea’s goals include Seattle Children’s becoming a center […]
Sleep is an important part of physical and mental health, especially in school-age children and adolescents. A well-rounded sleep schedule supports healthy brain function, maintains physical and emotional balance and reduces the risk of long-term health problems. Unfortunately, about 30% of parents say their kids are not getting enough shut-eye. While sleep challenges vary, research […]
Over the past 18 months, members of the Seattle Children’s Sickle Cell Disease Program has continued working diligently to improve and enhance care for children, teens and young adults with sickle cell disease (SCD) by expanding services, hours, and staffing, with a special focus on hiring a diverse team that represents the nearly 150 patients […]
In August 2020, just after her third birthday, Aisley began to experience concerning symptoms: headaches in the back of her head, a lack of appetite and vomiting. After a visit to her pediatrician, Aisley was sent to Seattle Children’s for an urgent neurology visit, where she passed the exam with “flying colors,” showing no signs of trouble. Still, Dr. […]
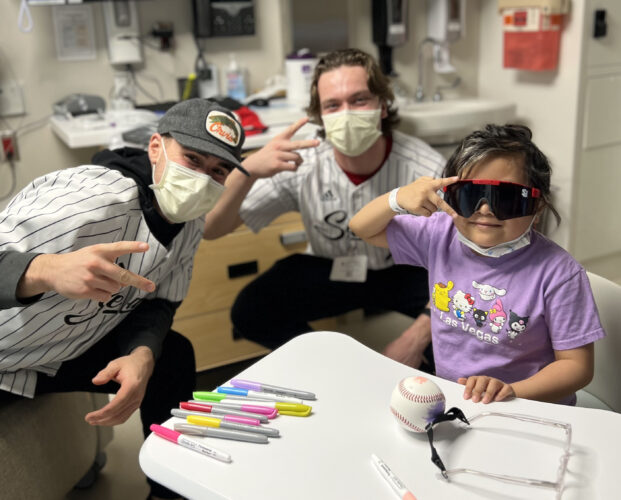
Baseball teams from the University of Washington and Seattle University helped Seattle Children’s patients ring in 2024 with two surprise visits to the hospital in January.
Families planning a home renovation or remodel should be aware that the walls they plan to tear down could contain hidden dangers that can hurt unborn babies and children’s growing bodies. Dr. Sheela Sathyanarayana is a pediatric environmental health specialist at Seattle Children’s Research Institute, and she says that people considering home renovations or remodels, […]
This article was originally published on the JAMA Network by Dr. Molly Taylor, an attending physician for Seattle Children’s Cancer and Blood Disorder Center and a researcher who runs the Biobehavioral Oncology Research Program in the Ben Towne Center for Childhood Cancer Research at Seattle Children’s Research Institute. [Content warning: Please be aware this article discusses grief and loss. Support […]
This holiday season, parents, caregivers, family and friends may be on the lookout for special gift ideas for the children in their lives. With so many choices available in person and online, it can feel overwhelming to find something that is both fun and safe. Depending on a child’s age, there are certain toys with […]
The halls of Seattle Children’s are decked with holiday cheer after patients and families were surprised by a special visit from a group of Pacific Northwest Ballet dancers hoping to spread happiness throughout the hospital. The dancers spent time with patients, handed out holiday-themed gifts and read The Nutcracker aloud. The ballerinas also decorated ballet […]